Understanding How Your Diet Affects Diverticulitis Flare-Ups

Introduction
Did you know that your choice of food can significantly affect your digestive health and potentially lead to diverticular flare-ups? Understanding the connection between diet and diverticulitis is essential for managing and preventing painful episodes. This guide provides clear insights into how dietary adjustments can influence this condition.
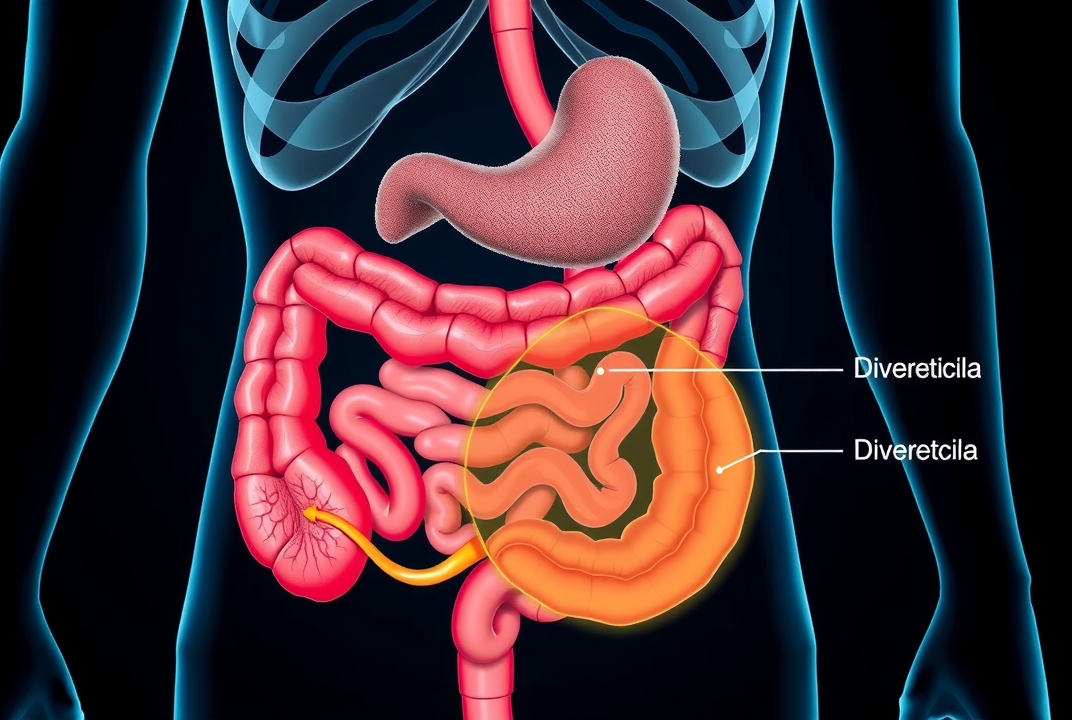
What is Diverticulitis?
Diverticulitis is a condition where small bulging pouches, known as diverticula, form in the digestive tract and become inflamed or infected. This can lead to severe abdominal pain, fever, and digestive complications.
The Role of Diet in Diverticulitis Flare-Ups
A crucial factor in managing diverticulitis is understanding the relationship between your diet and flare-ups. Consuming a fiber-rich diet is often advised to prevent the formation of diverticula or reduce symptom severity. Fiber helps bulk up the stool and aids in its smooth movement, minimizing pressure in the colon.
Carbohydrate and Fiber Intake
Fiber is a critical component of dietary management for diverticulitis. High-fiber foods such as whole grains, fruits, and vegetables contribute to maintaining good digestive health. However, during flare-ups, it may be necessary to switch to a low-fiber diet temporarily to reduce bowel irritation.
-
Choose oatmeal, bananas, or cooked carrots as gentle options during a flare-up.
Protein and Fat Considerations
Moderate your intake of red meats and high-fat foods, which may exacerbate symptoms. Lean proteins like chicken or tofu are preferable. Incorporate healthy fats from sources like olive oil or avocados.
Common Triggers and Foods to Avoid
Identifying and avoiding common dietary triggers can help manage symptoms. Certain foods might worsen symptoms for some individuals, although this can vary widely.
-
Seeds and Nuts: Previously thought to exacerbate flare-ups, recent studies show they are generally safe, though individual tolerance levels vary.
-
Processed Foods: Foods high in sugars and refined carbohydrates can lead to inflammation.
Nutritional Strategies for Managing Diverticulitis
A balanced approach can reduce the frequency and intensity of flare-ups. Here are some strategies:
Regular Meal Patterns
Regular eating patterns help in stabilizing digestion. Avoiding large meals can reduce stress on the digestive system.
Hydration
Maintaining adequate hydration supports intestinal function and eases the transit of food through the digestive tract.
Probiotics and Prebiotics
Including probiotics can support a healthy gut flora, potentially reducing symptoms. Foods like yogurt with live cultures or fermented vegetables are beneficial.
Expert Insights
Nutritionists often emphasize a tailored approach to managing diverticulitis. As Dr. Jane Smith, a gastroenterologist, suggests, "Understanding your body’s response to different foods is key to managing this condition effectively." Keeping a food diary may also be helpful to pinpoint individual triggers.

Conclusion
The link between diet and diverticulitis flare-ups is undeniable, with proper nutritional strategies playing a crucial role in symptom management. By consciously modifying your dietary habits, you can gain better control over symptoms and improve overall digestive health. Consider consulting a healthcare provider or dietitian for a personalized plan to navigate dietary choices effectively. Your digestive wellness is largely in your hands, manageable with informed dietary decisions.