Diverticulitis Flare-Up Symptoms: Myths vs. Facts
Introduction: Unpacking the Myths around Diverticulitis Symptoms
When it comes to diverticulitis, a surprising number of myths cloud the symptoms associated with flare-ups. This confusion can often lead to misdiagnosis and inappropriate management of the condition. Understanding the true symptoms of a diverticulitis flare-up is not only essential for proper treatment but also for improving overall health. In this article, we aim to clarify the differences between myths and facts about diverticulitis symptoms and provide a reliable guide for those seeking to better understand this common digestive condition.
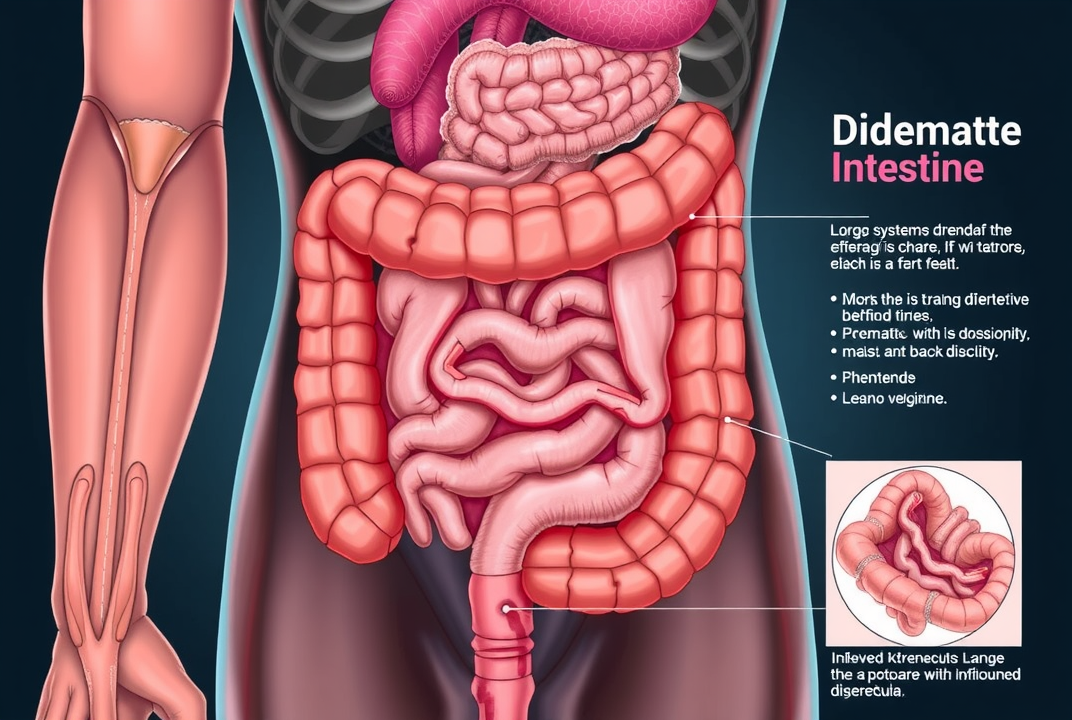
What is Diverticulitis?
Before exploring the symptoms, it's important to understand what diverticulitis is. Diverticulitis occurs when diverticula, small bulging pouches in the digestive tract, become inflamed or infected. This condition mostly affects the large intestine and can lead to various symptoms.
Myth 1: Diverticulitis Always Causes Severe Pain
Fact: While many people with diverticulitis experience abdominal pain, its intensity and location can vary. Some may encounter mild discomfort, while others suffer severe pain. The myth that diverticulitis always results in extreme pain can cause unnecessary fear and anxiety.
Myth 2: Diverticulitis Is Easily Diagnosed
Fact: Diagnosing diverticulitis is not always straightforward. Often, symptoms can mimic other gastrointestinal issues like irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD). Diagnosis usually requires medical imaging and sometimes colonoscopy to confirm.
Image Placement Suggestion
Myth 3: Diet Does Not Affect Diverticulitis Symptoms
Fact: Diet significantly impacts the symptoms and management of diverticulitis. High-fiber diets are encouraged to prevent the formation of diverticula. During a flare-up, a low-fiber diet is usually recommended to reduce irritation.
Myth 4: Only Older Adults Get Diverticulitis
Fact: Though more common in people over 50, younger adults can also develop diverticulitis. Factors such as lifestyle, diet, and genetics play roles in its occurrence across various age groups.
Discussing Common Symptoms
Understanding the actual symptoms of a diverticulitis flare-up provides clarity and aids effective management:
-
Abdominal Pain
-
Often located on the lower left side of the abdomen, manageable with medication.
-
-
Bloating and Gas
-
Common but not always associated with severe discomfort.
-
-
Fever and Chills
-
Indicative of infection, needs medical attention.
-
-
Nausea or Vomiting
-
May accompany severe pain, often leads to reduced appetite.
-
Image Placement Suggestion
Myth 5: Surgery is the Only Treatment for Diverticulitis
Fact: Surgery is typically a last resort. Most cases are managed with antibiotics, dietary changes, and lifestyle adjustments. Early intervention can prevent the need for surgical procedures.
The Role of Medical Consultation
Consulting a healthcare professional when experiencing symptoms is crucial, given the complexity and potential severity of diverticulitis. A personalized treatment plan often includes:
-
Antibiotics to manage infections.
-
Dietary Adjustments to prevent further flare-ups.
-
Regular Monitoring to keep track of any changes or improvements.
Practical Tips for Managing Diverticulitis
-
Maintain a High-Fiber Diet (when not in a flare-up) to promote digestive health and prevent onset.
-
Stay Hydrated to support overall gastrointestinal wellness.
-
Avoid Triggers by identifying foods or habits that lead to symptoms.
-
Exercise Regularly to boost digestive functions and overall health.
Image Placement Suggestion

Conclusion: Separating Myths from Reality
Understanding the difference between myths and facts about diverticulitis flare-up symptoms plays a vital role in managing the condition effectively. Through proper education and medical guidance, individuals can lead healthy lives without the misconception-driven anxiety linked to diverticulitis. If you suspect symptoms, consult with healthcare professionals to receive accurate diagnosis and appropriate care.