Understanding IBS vs. Diverticulitis: Key Differences and Symptoms
Introduction
Did you know that up to 60 million individuals in the United States experience digestive disorders? Irritable Bowel Syndrome (IBS) and Diverticulitis are two prevalent conditions that can cause discomfort. Understanding these conditions is crucial as their symptoms often overlap, but the implications and management strategies differ. This article will guide you through distinguishing between IBS and Diverticulitis, empowering you to make informed health decisions.
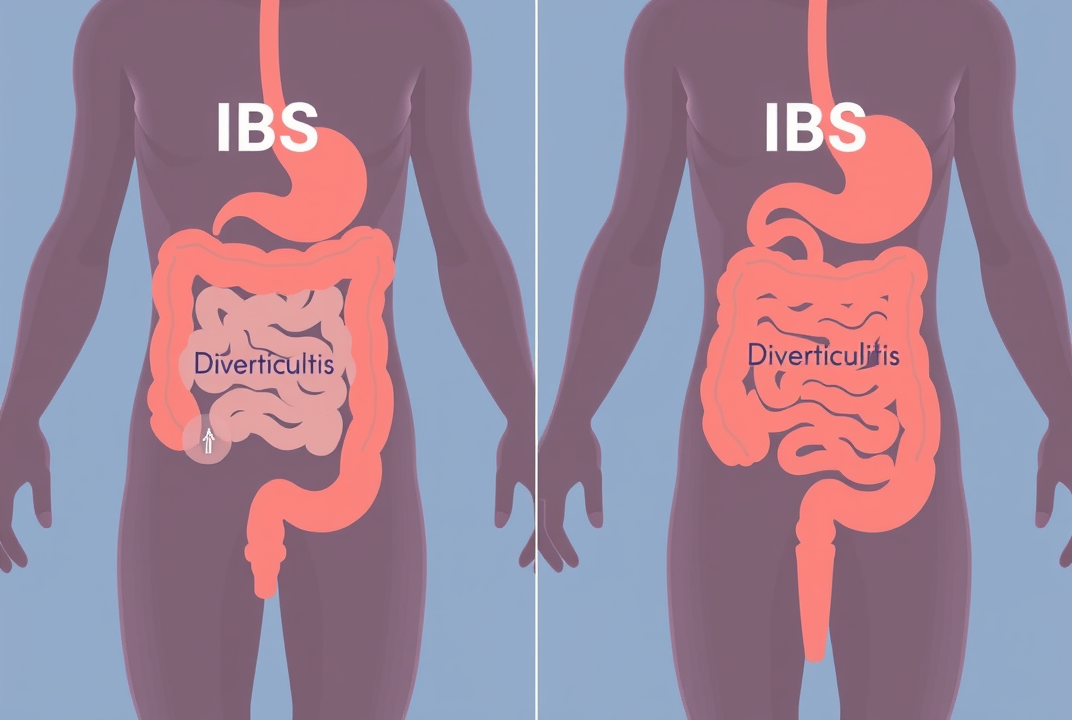
What is Irritable Bowel Syndrome (IBS)?
IBS is a functional gastrointestinal disorder characterized by abdominal pain, bloating, and changes in bowel habits, without any visible signs of damage or disease in the digestive tract. It often causes persistent discomfort and can have significant impacts on daily life.
Symptoms of IBS include:
-
Abdominal pain or cramping
Bloating and gas
-
Diarrhea or constipation, or alternating between both
Mucus in the stool
The exact cause of IBS is not fully understood, but factors such as gut-brain interaction, stress, and diet may play significant roles. Diagnosis usually involves ruling out other conditions with similar symptoms.
What is Diverticulitis?
Diverticulitis occurs when small, bulging pouches (diverticula) that can form in the lining of the digestive system become inflamed or infected. This condition is more common in individuals over 40.
Symptoms of Diverticulitis include:
-
Severe abdominal pain, usually on the left side
Fever and chills
Nausea and vomiting
-
Changes in bowel habits (constipation or diarrhea)
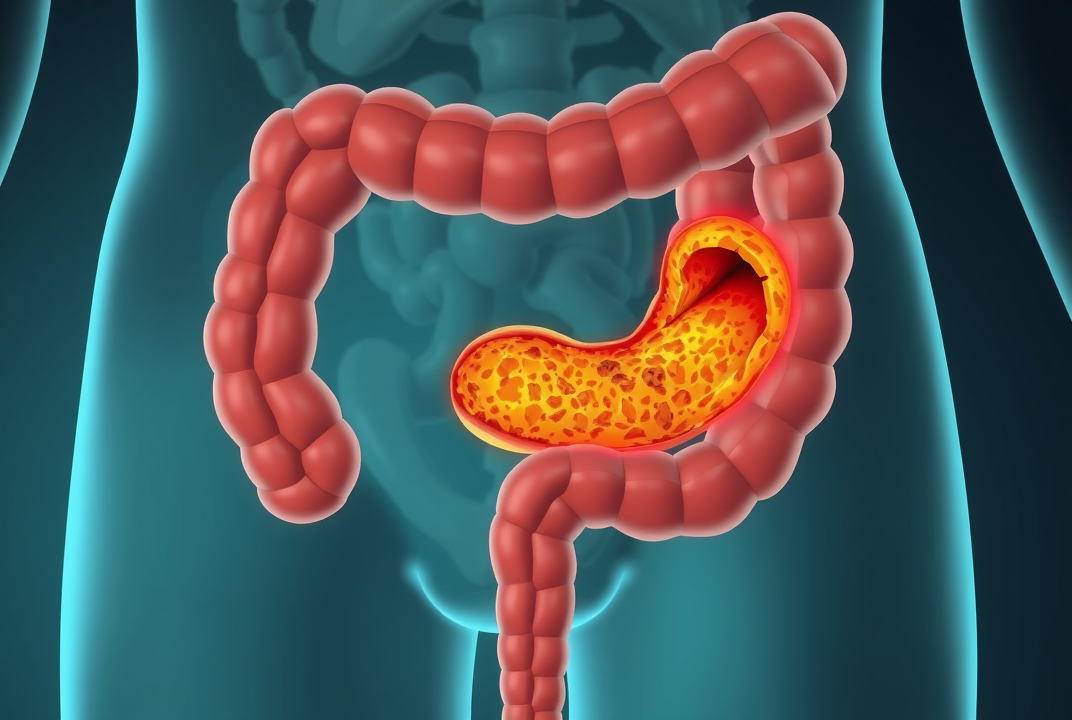
The exact cause of diverticulitis is also unclear, but factors like aging, low fiber diet, and lack of exercise are often linked. Diagnosis might require CT scans or other imaging tests to identify inflamed sites.
Key Differences Between IBS and Diverticulitis
-
Nature and Cause:
-
IBS: A functional disorder affecting how the gut functions without specific physical damage.
-
Diverticulitis: Physical condition involving inflammation of pouches in the digestive tract.
-
-
Symptoms:
-
IBS: Often involves recurrent abdominal pain with bloating and changes in bowel movements without fever.
-
Diverticulitis: Typically includes localized severe pain, fever, and sometimes nausea.
-
-
Age and Risk:
-
IBS: Can occur at any age but often starts in early adulthood.
-
Diverticulitis: More common as people age, particularly after 40.
-
-
Diagnosis:
-
IBS: Based largely on symptom patterns; no definitive test.
-
Diverticulitis: Identified through imaging tests like CT scans.
-

Treatment Options
For IBS:
-
Dietary Adjustments: Reducing intake of trigger foods (such as dairy or fried foods) can help manage symptoms.
-
Medications: These may include laxatives, anti-diarrheal drugs, or prescription medications to relieve pain.
-
Stress Management: Techniques like mindfulness and regular exercise can be beneficial.
For Diverticulitis:
-
Antibiotics: Used to treat or prevent infection.
-
Liquid Diet: Giving the gut a rest during the initial phase can reduce symptoms.
-
Surgery: In severe or recurrent cases, surgery may be needed to remove the affected part of the intestine.
Prevention Tips for Digestive Health
-
Balanced Diet: Increasing fiber intake with fruits, vegetables, and whole grains.
-
Hydration: Drinking plenty of fluids helps maintain bowel function.
-
Regular Exercise: Promotes good digestion and reduces stress.
-
Routine Screening: Especially for adults over 40, to monitor digestive health.
Conclusion
Understanding the differences and similarities between IBS and Diverticulitis is vital for effective management and improved quality of life. While both conditions can cause significant distress, proper diagnosis and tailored treatment can transform lives. For those experiencing ongoing digestive symptoms, consulting with a healthcare provider is a crucial step towards clarity and control. Taking charge of your digestive health through lifestyle adjustments, and professional guidance can lead to a more comfortable and symptom-free life.