Questions to Ask Your Doctor About Diverticulosis and Diverticulitis
Introduction
Did you know over 50% of people over the age of 60 may develop diverticulosis? Understanding this common condition, along with its potentially serious counterpart, diverticulitis, is important for maintaining digestive health. Whether you've been recently diagnosed or have been managing these conditions for years, knowing the right questions to ask your doctor can make a significant difference in your treatment and quality of life.
In this article, we will explore the essential questions you should ask your healthcare provider. From understanding your symptoms and treatment options to managing your diet and lifestyle, these questions are designed to empower you.
Understanding Diverticulosis and Diverticulitis
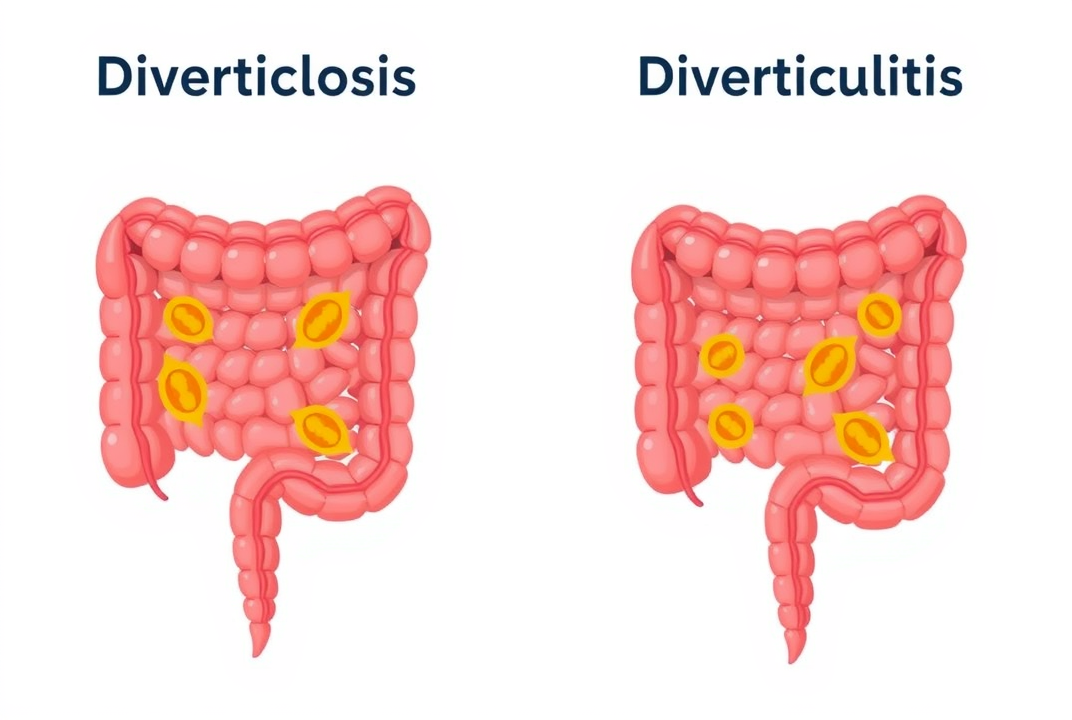
Diverticulosis involves the formation of small pouches in the colon wall, which may not cause symptoms. However, when these pouches become inflamed or infected, the condition is known as diverticulitis.
Key Differences
-
Diverticulosis: Generally asymptomatic. Detectable often through colonoscopy or imaging tests.
-
Diverticulitis: Symptoms may include abdominal pain, fever, and changes in bowel habits. Requires medical intervention.
Questions About Diagnosis
1. What are the indicators of diverticulosis or diverticulitis I should be aware of? Many individuals may not experience any symptoms with diverticulosis. However, symptoms like abdominal cramps, bloating, or irregular bowel movements might occur. For diverticulitis, symptoms usually include more acute abdominal pain, nausea, and fever. Understanding these indicators helps in early identification and management.
2. How are these conditions diagnosed and why are these methods chosen? Your doctor may recommend specific tests such as CT scans or a colonoscopy. Discussing the reasons for these methods would provide clarity on what to expect during the diagnostic process.
Treatment Options
3. What treatment options are available for diverticulosis and diverticulitis? Treatment varies significantly between the two conditions. Diverticulosis may not require invasive treatment and can often be managed with diet. For diverticulitis, antibiotics or surgery might be necessary, depending on the severity.
4. Are there any potential side effects of these treatments I should be aware of? Understanding possible side effects helps in planning and managing your treatment effectively. Discussing long-term implications and follow-ups can pave the way for better health outcomes.
Diet and Lifestyle Considerations
5. How should my diet change if I have diverticulosis or diverticulitis? Diet plays a crucial role in managing both conditions. High-fiber foods can prevent symptoms of diverticulosis, while a clear liquid diet might be recommended for diverticulitis.
6. Are there lifestyle changes that could help manage my condition? Regular exercise, managing stress, and staying hydrated are general recommendations that can positively impact your condition. Your doctor may have tailored advice based on your unique situation.
Monitoring and Follow-up
7. How often should I schedule follow-up appointments? The frequency of your follow-up visits relies on your condition's severity and treatment response. Regular check-ups are vital to monitor the disease's progression and adjust treatments when necessary.
8. What signs indicate that my condition is worsening or improving? Understanding which symptoms signal improvement or deterioration aids in self-monitoring and long-term management.
Psychological Impact and Support
9. How can I address the emotional and psychological aspects of living with these conditions? Coping with chronic conditions can be emotionally challenging. Seek counseling or support groups, which can offer valuable emotional support and coping strategies.
Conclusion
By approaching your doctor with these critical questions regarding diverticulosis and diverticulitis, you take an active step in your healthcare journey. Effective communication with your healthcare provider allows you to make informed decisions about your treatment and lifestyle adjustments, paving the way for better digestive and overall health.
Remember to schedule regular follow-ups, stay informed about your condition, and actively engage in conversations with your healthcare team. This proactive approach can significantly contribute to managing your condition effectively and enhancing your quality of life.